OTC

Unwelcome guests
In OTC
Bookmark
Record learning outcomes
Uninvited guests in search of free bed and board, such as head lice, scabies and threadworm, need to be addressed quickly in order to prevent entire households being infected

Learning objectives
After reading this article you will be able to:
- Identify the most common infestations in humans
- Help customers select the best treatment option
- Offer best practice advice on how to prevent reinfection
While head lice, scabies and threadworms may be very different from one another, a characteristic they share is the ability to make people feel uncomfortable, embarrassed and even distressed, something that is driven largely by the fear of what others around them might think.
“There is a stigma around these conditions [being linked to] cleanliness,” explains Dr Sweta Rai of the British Association of Dermatologists, “when, in fact, they are caught through close contact with [other] individuals. With the right treatments, however, these conditions can usually be cleared up quickly and completely.
“Good advice can provide an early diagnosis and prevent the condition getting worse and associated eczema-like skin changes and secondary infections of the skin from developing, which can occur in untreated scabies and head lice.”
Ian Burgess, director of the Medical Entomology Centre at Insect Research and Development Limited, stresses that when it comes to spotting conditions such as scabies or threadworms (which often go undiagnosed), education is crucial. “In many cases, you’ll find that people have gone on the internet and opted to self-diagnose, which often leads to self-medication. Pharmacy staff need to be able to pick up on these medication requests and take the opportunity to suggest a consultation with the pharmacist.
“Similarly, pharmacy staff need to be able to recognise the classical signs of a condition such as scabies, while understanding such pointers might actually be a lot more subtle than they might think. The reason for this is simple – greater levels of cleanliness mean that people are sloughing off a lot more skin than they used to, so scabies won’t be as obvious. We can see this through the size of scabies burrows now, which often are not more than 2mm even if you do manage to find one. In the past, you would have been looking for 1-3cm burrows.”
Another challenge that pharmacists and their teams habitually face when treating infestations is the need for the patient to adhere to the product instructions. “Instructions for use come with the medication,” Dr Rai points out, “and it is important that people understand that these should be followed to the letter and that everyone in the family should be treated simultaneously, whether they are experiencing symptoms or not, otherwise they run the risk of catching it again, which is quite common.”
This tendency to skip steps or fail to complete treatment is often seen in the case of head lice, says Ian Burgess, with people either failing to use a product properly or opting for something that isn’t up to the job – in the case of a nit comb, for instance. “The problem with treatments for head lice is that they are often more difficult to use correctly than you might think, so you’ll find people coming back and saying that something didn’t work when, in fact, they have failed to use a product properly or simply haven’t put in the time needed.”

Recommending treatments
Head lice
What are head lice?
Head lice are common in children between the ages of four and 11 years – particularly girls. Although children are more typically affected, head lice will live on anyone’s scalp, which makes the whole family susceptible.
While head lice have, at times, been associated with poor hygiene, in reality they will make their home in any human hair and at any time of the year.
How do you recognise them?
Head lice are tiny grey-brown insects (see above) that live on human scalps. They cannot be caught from animals. Unable to fly or jump, these sesame seed-sized insects are instead transferred by close contact – such as head-to-head touching, which is why children are often the target.
Pharmacy staff need to be able to pick up on these medication requests and take the opportunity to suggest a consultation
Symptoms can include an itchy scalp from lice bites, saliva and faeces, although Ian Burgess points out that numerous studies have not found this to be common. However, signs of a long-term infestation may present as:
- Sore scalp (due to the same bacteria that cause impetigo)
- Raised temperature and general feeling of unwellness
- Scratch marks or a sticky weeping scalp
- Small itchy pink bumps around the edge of the scalp, particularly on the back of the neck
- Enlarged glands in the neck.
Tips for diagnosis
Detection combing is the most efficient means of accurately diagnosing the presence of head lice and the mainstay of any prevention regimen, says Burgess.

Treatment options
Treatment is only needed if an active louse infestation is present and detected. There are three options, which are all available on general sale:
- Physical insecticides (e.g. dimeticone and other synthetic oily products) work by physically coating the surfaces of head lice and disrupting their water balance, causing suffocation
- Chemical insecticides (e.g. permethrin 1% creme rinse; malathion 0.5% liquid). These formulations are neurotoxic poisons for the head lice but widespread resistance has been reported so they can be ineffectual
- Wet combing: Lubricating the hair with a conditioner or a product containing silicones or other suitable cosmetic oils makes wet combing easier and more effective. The comb should be wiped on white paper or cloth after each pass to remove lice and eggs. More information on wet combing is available via Community Hygiene Concern (chc.org).
Wet combing or dimeticone 4% lotion is generally recommended as the first-line treatment for women who are pregnant or breast-feeding, young children (aged six months to two years), and people with asthma or eczema.
Back to school...
Dermatologists are warning that, with the new school year now underway, many parents will find their children are bringing home more than just homework.

The start of classes tends to mark the start of head lice season, as lice previously confined to small networks over the summer spread from child to child, says the British Association of Dermatologists. Pharmacists can give the following simple steps to parents to help them prepare for and manage an outbreak:
- Make sure that you have the essentials at home already – a large bottle of conditioner and a nit comb
- Check for nits pre-emptively at home using a nit comb to identify infestation early. Prompt treatment helps prevent further spread
- If you do find evidence of nits, get to work with the nit comb. Lubricating the hair with a generous amount of conditioner to wet hair will make the procedure easier, particularly for curly hair. You should then comb through all the hair from the roots to the ends. Depending on the hair type and length, the wet combing process can take up to 45 minutes
- The comb must be cleaned immediately after each pass to remove lice and eggs. This is best done by wiping on clean white paper or cloth
- Check family members for head lice. Parents should keep in mind that head lice can spread to anybody, no matter how clean their hair or home is, Holly Barber of the British Association of Dermatologists points out
- To ensure all head lice are removed, repeat the wet combing process two or three times within the first two weeks following infestation
- Continue to check for head lice every week for a month to ensure that they have not returned.
Scabies
What is scabies?
Scabies is caused by tiny parasitic mites, Sarcoptes scabiei, laying eggs inside the epidermis. Children tend to be the most common group affected, which puts everyone in the household at risk. Scabies is not usually serious but will need to be treated. The symptoms may take up to eight weeks to appear and this asymptomatic period is the time people are most infectious.
Scabies
Scabies is always spread by direct skin-to-skin contact with someone who already has the condition. Any link to sharing clothing, towels or bedding is a myth, says Ian Burgess. Scabies on pets is caused by a different type of mite and cannot infect humans.
Key symptoms
- If burrows are discovered, scabies mites may appear as silvery lines with a dot at one end
- A rash – typically mild, barely coloured and transient, this is commonly overlooked. According to Ian Burgess, it mostly affects the midriff, the insides of the thighs, and lower legs. The rash may also appear on elbows, lower legs and feet, under breasts, and on the buttocks and scrotum
- A secondary rash that is associated with the sites where mites are found occurs mainly in the webs of skin between the fingers and toes, wrists, ankles, groin and breasts. (It is important to note that very young children and the elderly with poor immune competence may well develop a rash on the head too, with infants sometimes displaying a rash on their palms or soles.)
- Itching often becomes worse at night
- Scabies can present as red spots and scratches, but scratched areas may develop into crusty sores, which can become infected and develop into small pus spots. A widespread rash similar to eczema (dermatitis) is very common.

Treatment options
Permethrin 5% cream and malathion 0.5% liquid are common treatments in the UK and are available as OTC products. Both options should be cross-checked before sale, however, as both are also useful for head lice. Benzyl benzoate emulsion is an alternative and, although not as cosmetically acceptable, it may be effective if other treatments fail. A GP may suggest different preparations for babies or women who are pregnant or breast-feeding, so a referral may be necessary.
Tips for application
- Any treatment should be applied from top to toe in adults and children (even non-itchy areas, including the scalp)
- Cream or lotion should be left on for at least 12 hours before being rinsed off (customers should be reminded to re-apply when hands are washed during this period)
- Two treatments, one week apart, will be necessary to kill mites that have hatched out from the eggs after the first application.
Additional advice
Everyone in the household needs to be treated at the same time, even if they do not have symptoms. Following treatment, bed linen and clothing may be laundered as usual.
Threadworms
Commonly known as threadworms or pinworms, these tiny parasites live in the large intestine. They are common in children and spread easily, but are straightforward to treat with medication and hygiene measures. Usually emerging from the anus at night, threadworms are between 10-13mm long and can sometimes be seen around this area with the aid of a torch. A female worm will live for five to six weeks before laying her eggs around the anus and dying.
Symptoms
- Threadworms may be visible as tiny white threads in the faeces
- Severe itching around the anus (and sometime the vagina in girls, when worms have emerged and made their way across the perineum). This itching is usually worse at night or in the early morning, when the mucus around the eggs has dried out
- Irritability and waking up during the night
- Less common signs may include weight loss, wetting the bed and irritated skin around the anus.
Treatment options
Mebendazole is the only treatment licensed and is usually taken in the form of a two-step chewable tablet. However, if treating a child under two years of age, or in the case of a woman who is pregnant or breastfeeding, a GP should be consulted.
Important advice
- Medication will treat the worms but not any eggs that may have been laid – so strict personal and household hygiene measures are recommended for two weeks after treatment
- Everyone in a household should be treated if threadworms are detected, even those without symptoms
- Most infection comes from inhalation, so regularly washing bedclothes (but not shaking out bedclothes, pyjamas or nightdresses), and performing a regular household clean by damp-dusting and vacuuming is recommended
- Ensure children wear underwear at night and change it every morning
- Everyone should wash their hands regularly, brush under nails, and rinse toothbrushes before use.
Rare infestations
Although mainly seen in tropical locations, the following parasitic infections may well present in pharmacies in the UK as a result of foreign travel. If you suspect a person may have contracted any of the following, refer them to a GP immediately:
Amoebiasis (amoebic dysentery)
An infection of the intestine with amoeba, amoebiasis is picked up as a result of ingesting contaminated water. There are several different types of amoebic infection, most of which are asymptomatic. If there are any symptoms, these can vary in severity, with the most serious caused by an amoeba called Entamoeba histolytica that can cause severe diarrhoea with blood.
Other symptoms associated with amoeba may include:
- Frequent loose stools
- Abdominal pain
- Cramps
- Fatigue
- Intermittent constipation
- Diarrhoea with abdominal swelling
- Flatulence.
Amoebic dysentery is treated with metronidazole or tinadazole.
Giardiasis
An infection in the small intestine caused by a microscopic parasite called Giardia lamblia, giardiasis is caught through faecal-oral contact with infected people, by eating or drinking contaminated food or water, touching surfaces that have been contaminated by an infected person and then putting fingers in the mouth, or handling finger food.
Although cases are fairly uncommon, there have been some notable outbreaks. The main symptoms are smelly diarrhoea, tummy pain or cramps, flatulence, belching, bloating and weight loss. The infection can be treated with metronidazole or tinadazole, so an urgent GP consultation is recommended. If the customer is dehydrated, oral rehydration sachets should be also recommended.
Schistosomiasis
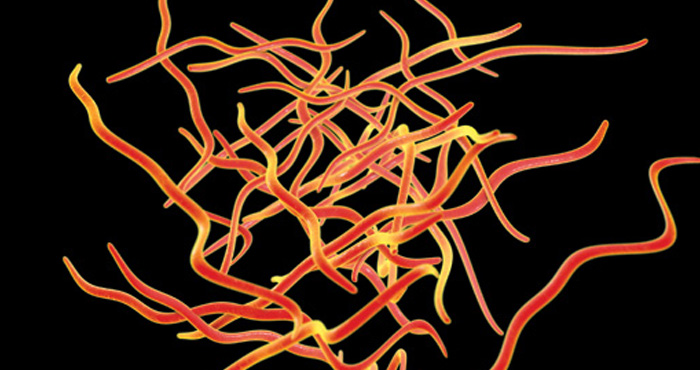
Schistosoma mansoni and Schistosoma japonicum are worm parasites endemic to parts of Africa, South America, the Caribbean and parts of Asia. The adult worms are resident in the hepatic portal vein, producing spined eggs that may get trapped in the liver, venous and gut wall tissues as they work their way out into the gut lumen and cause granulomas in those tissues.
Schistosoma haematobium lives in the blood vessels around the bladder and the eggs cause blood leakage into the bladder on their way out. They cause granulomas where they become trapped in the bladder wall and the urethra.
Most short-term travellers will never show symptoms. Those who will show signs are people who are infected repeatedly over long periods, or who have been exposed to the infective cercaria stage while swimming or paddling in infested waters.
