Bladder weakness
In OTC
Follow this topic
Bookmark
Record learning outcomes
Bladder weakness remains a taboo subject – so how can you help raise awareness without causing any additional embarrassment?
Learning objectives
After reading this feature you should be able to:
• Appreciate the extent of bladder control problems and their impact on quality of life
• Raise awareness of available help and support
• Recommend lifestyle changes and self-care measures to help manage symptoms
Around 14 million people in the UK have some form of bladder leakage (urinary incontinence) and, despite common belief, both men and women – young and old – can be affected. The biggest challenge is encouraging people to seek help about such a taboo topic, with many too embarrassed to mention it to their GP and buying incontinence products to cope with any leakage instead.
Urinary incontinence can have a significant impact on quality of life, yet many people consider it to be a normal part of ageing and are unaware that it can be treated. Rizwan Hamid, consultant urologist at the Princess Grace Hospital (part of HCA Healthcare UK), says incontinence is a symptom rather than a disease or diagnosis and needs to be taken seriously.
“There’s a perception that there aren’t any treatments available, but this isn’t the case,” he says. “Treatments range from lifestyle measures and pelvic floor exercises to medication and surgery, depending on the cause. All patients should be encouraged to seek help from a healthcare professional.”
Types of incontinence
The main types of urinary incontinence seen in primary care include:
- Stress incontinence: accidental urinary leakage associated with pressure on the bladder due to exercise, laughing, coughing, lifting heavy items or sneezing. This is often due to weak pelvic floor muscles
- Urge incontinence: leakage with, or just after, an intense sudden urge to pass urine, especially at night. This is often associated with an overactive bladder, which is when the bladder muscles are more sensitive or active than usual
- Mixed incontinence: a mixture of both stress and urge incontinence
- Overflow incontinence (chronic urinary retention): when the bladder doesn’t fully empty and urine leaks out, usually due to a blockage or obstruction.
Anyone experiencing bladder leakage should keep a diary for a few days to help identify any specific triggers or causes. They should record how much fluid they drink each day, how much and how often they urinate, and if or when they have any bladder leakage (and how much).
Common risk factors
Women during and after pregnancy or around the menopause may be at an increased risk of urinary incontinence due to weaker pelvic floor muscles. These muscles help to support the bladder, bowel and uterus. Pelvic prolapse (when one or more of the pelvic organs slips out of position and bulges into the vagina) may be associated with both bladder and bowel symptoms.
According to a 2019 NICE guideline on the management of urinary incontinence and pelvic prolapse in women in primary care, 8.4 per cent of women report a vaginal bulge or lump and on examination prolapse is present in up to 50 per cent.
Not all urinary leakage is associated with pelvic or bladder problems, however. Increased production of urine may be associated with diabetes or a problem with the kidneys, for example. Obesity and other lifestyle factors also play an important role in the development of urinary incontinence.
In February 2020, researchers at Glasgow Caledonian University found a direct link between sitting for too long and urinary incontinence in older women. “We found that women who had urgency incontinence sat for significantly longer periods than the women with no incontinence – about 19 per cent longer than the rest – so there is a clear link between sitting and having urgency urinary incontinence,” says Professor Joanne Booth, lead author of the research paper. “Irrespective of how old you are or how heavy you are, if you sit for about a fifth longer than an average of 18 minutes you are more likely to have an overactive bladder.”
Incontinence is widely seen as a female problem, affecting twice as many women as men. However, male continence shouldn’t be overlooked. Men are more likely to develop bladder problems as they get older, due to prostate gland enlargement or after prostate surgery. Benign prostatic hyperplasia causes lower urinary tract symptoms (needing to pass urine frequently, trouble starting to urinate and loss of bladder control) and affects around a third of men over the age of 50 years (see below).
Most urinary incontinence isn’t due to serious disease but very occasionally it can be due to an obstruction, infection, tumour or interstitial cystitis (painful bladder syndrome). Other possible causes include neurological conditions (e.g. Parkinson’s disease), some connective tissue disorders (such as Ehlers-Danlos syndrome) or certain medicines (e.g. ACE inhibitors and some antidepressants).
Management approaches
The first step in managing urinary incontinence in men and women is to do a lifestyle assessment and make appropriate changes if necessary. According to NICE guidance, women with an overactive bladder should reduce their caffeine intake as caffeine can irritate the bladder and increase urine production. Women with urinary incontinence or an overactive bladder should also look at their fluid intake (both too much and too little fluid can make urinary incontinence worse). They should lose weight if their BMI is more than 30 and stop smoking if they smoke.
Pelvic floor exercises (at least three times a day for at least three months) are a first-line approach for women with stress or mixed urinary incontinence. Many women don’t know how to do these exercises properly but GPs can refer them to a specialist continence physiotherapist for an individual exercise programme.
“Pelvic floor exercises are often an easy and effective way of starting to manage symptoms of urgency and leakage, as well as assisting bowel control issues,” says Liz Kirton, clinical specialist physiotherapist in pelvic health at the Portland Hospital.
“The NHS ‘Squeezy’ app for pelvic floor exercises may be something to recommend to pharmacy customers. We would always recommend seeing an experienced pelvic health physiotherapist for any conditions related to the pelvic floor area, so knowing referral routes or availability in the local area may be very beneficial for pharmacy customers.”
Women with urge or mixed incontinence should be offered bladder training for a minimum of six weeks. Bladder training involves learning how to wait longer between feeling the need to urinate and passing urine, guided by a specialist. It may be combined with pelvic floor muscle training. If frequency is a troublesome symptom and bladder training doesn’t work on its own, women should be offered anticholinergics for an overactive bladder.
Men with urinary incontinence may also benefit from supervised pelvic floor exercises and bladder training, alongside lifestyle changes (e.g. fluid intake). If these measures don’t help, men may be offered medication (e.g. anticholinergics) or intermittent self-catheterisation. If overflow incontinence is caused by an enlarged prostate, doctors may recommend prostate surgery.
Pharmacy intervention
Incontinence pads, pants and other products (e.g. shields for men) are not a treatment for urinary incontinence but can help pharmacy customers cope with leakage. According to Mintel’s report, Feminine Hygiene and Sanitary Protection Products – UK (February 2020), the feminine hygiene and sanitary protection category has seen gradual growth in recent years. “The incontinence sector remains the engine behind this growth, benefiting from the UK’s ageing population, as well as heavy advertising expenditure giving rise to stigma-tackling campaigns.”
According to Liz Kirton, community pharmacists are well placed to discuss continence issues with customers. “The phrase ‘common, not normal’ is regularly used for describing continence issues,” she says. “Notice when patients are purchasing items such as continence pads – or menstrual pads when in an age range unlikely to need them – or regularly purchasing products to assist the reduction of urinary tract infections, such as cranberry preparations. Having some literature freely available and visible may also be beneficial in opening conversations and signposting customers.”
According to the Mintel report, many women continue to use sanitary protection for incontinence. Emphasising the benefits of dedicated incontinence products, such as odour control and absorption rate, is key to encouraging them to switch products. Men are just as likely to buy incontinence products online as they are to purchase them in-store. Mintel suggests retailers (or pharmacies)could place products in more discreet areas of the store or closer to tills, while brands could consider making packaging more discreet.
Pharmacies often stock pelvic floor toners, weights or electrical stimulation units to improve pelvic floor muscle strength but customers should be assessed by an experienced specialist physiotherapist before they buy a device, says Liz Kirton. “Some gadgets can be extremely costly and are not always appropriate,” she says. “Some toners are available on prescription, such as the PelvicToner and Kegel8 Weights. If a customer attends the pharmacy requesting these, it would be another opportunity to ask if they need assistance.”
Skin care advice is also important as chronic urinary incontinence can lead to skin irritation and fungal infections. Barrier creams can help to stop the skin becoming dry and inflamed.
Bladder problems in children
Many young children wet the bed at night and parents often think that this is normal. However, nocturnal enuresis is considered to be a medical condition once a child reaches five years of age. According to ERIC (the children’s bladder and bowel charity), around half a million children and young people in the UK experience nocturnal enuresis – one in 17 seven-year-olds and one in 75 teenagers. Some of these children may have daytime wetting and/or constipation as well.
Nocturnal enuresis can have a deep impact on children’s behaviour, emotional wellbeing and social life. Dr Feilim Murphy, consultant paediatric urologist at the Portland Hospital, stresses the term ‘bedwetting’ should be avoided as it causes confusion and stigmatisation. “The most sensible way to manage nocturnal enuresis in children is to understand the causes,” he says. “Parents and children need support to understand there is help and they can get better.”
June Rogers, children’s specialist nurse at Bladder & Bowel UK, says all children who are wetting the bed should have a proper bladder and bowel assessment. “There are two main causes of nocturnal enuresis – the overproduction of night-time urine or the inability of the bladder to store urine,” she says. “This could be due to constipation and/or an overactive bladder. All children with problems with bedwetting will probably not [be] waking in the night to go to the toilet. Children who wet the bed may also have a lack of vasopressin, the hormone that triggers the kidneys to produce less urine at night.”

Lifestyle advice
Lifestyle changes may help in some cases. “Parents should make sure their child drinks enough fluid throughout the day – 1,500ml, around six drinks,” she says. “Children need to urinate regularly during the day and before they go to bed. Suggest avoiding, or cutting down on, caffeinated or fizzy drinks, such as tea, coffee and cola. Children also need easy access to the toilet at night.”
If these measures don’t work after six weeks, parents will need to try other approaches. According to NICE guidance, a bedwetting alarm can be offered as a first-line treatment although this can take four to six months to work. Desmopressin (to replace vasopressin) may be offered to children over seven years, if it is appropriate.
Urinary tract infections can cause incontinence and may be associated with constipation. According to Dr Murphy, oral antibiotics should be prescribed, along with suitable painkillers to ease pain and lower any fever. “The most important next step is to ensure that there is daily soft bowel action and adequate fluid intake,” he says. “Oral laxatives are important in ensuring the presence of a soft regular bowel action. There is evidence that regular cranberry capsules with A-type proanthocyanidins are beneficial, and increasing evidence that D-Mannose is of some benefit, but large-scale randomised trials are only just starting.”
Prostate cancer: Know the early warning signs
Prostate cancer is the most common cancer in men with nearly 40,000 diagnoses every year in the UK – and loss of bladder control could be an early sign. Saheed Rashid, managing director, BXTAccelyon, discusses some of the first warning signals of this cancer and the potential side-effects of the various treatments
Over the past FEW YEARS, well known personalities such as Bill Turnbull and Stephen Fry have shared their experiences of prostate cancer, which has led to more men getting themselves checked – but many still remain unaware of the early symptoms, particularly around the loss of bladder control.
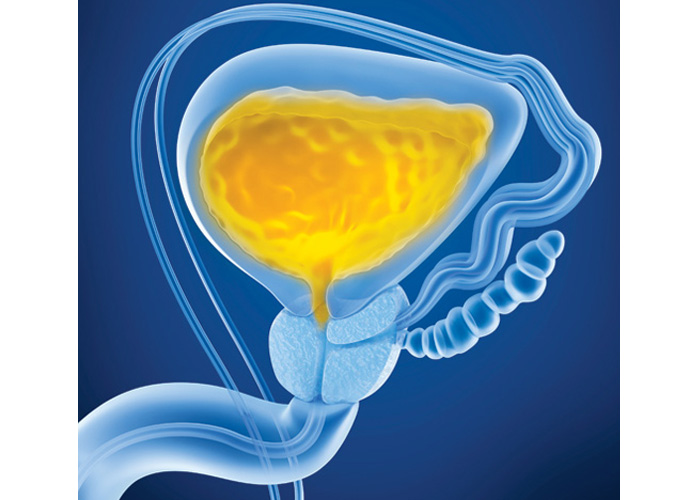
Signs and symptoms
Typically, prostate cancer occurs in older men, with the average age at diagnosis being around 66 years. Different men have different symptoms. While some men do not experience any symptoms, especially in the early stages, many early warning signs are linked to a loss of bladder control. This more commonly occurs when the prostate is large enough to affect the urethra, the tube that carries urine from the bladder out of the penis, which can increase the need to urinate, while having difficulty in starting to pass water or the feeling that the bladder has not emptied fully.
These symptoms should not be ignored or brushed aside as ‘just as part of getting older’. However, men must also keep in mind that these signs do not necessarily mean that they have prostate cancer and could be caused by other conditions, such as a prostate infection or reactions to medications. However, by having an increased knowledge of these particular symptoms of prostate cancer, men can double check these concerns with their GP or pharmacist if they experience any unusual feeling when urinating.
PSA testing — case study
David Robb, a 69-year-old retired school teacher from Scotland, experienced lower urinary tract symptoms (LUTS) over a three-year period with an increased need to urinate, which often became uncontrollable. Over this period of time, he was provided with medication by his doctor to try and control his urine, and had his PSA (prostate-specific antigen) level monitored.
The PSA test screens for prostate cancer and is available free to any man aged over 50 years who requests it after careful consideration of the implications. Typically, but not always, the higher the PSA level in the blood, the more likely a prostate problem is present. It can therefore be helpful to establish a baseline PSA level to help monitor variation over time, which is what David was able to do.
From his first check in January 2017 to July 2019, his score had risen by 0.4, which is when he was referred for further investigation and diagnosed with prostate cancer. Fortunately, his confirmed cancer was contained on one side of the prostate and was at an early stage of progression, meaning it was treatable without too many problems. But by noticing these symptoms and getting them checked early, David was able to have the cancer successfully treated and maintain his quality of life.
This highlights the importance of encouraging men to go to their pharmacist or GP to discuss any concerns, particularly regarding urination problems – or indeed encouraging them to get their baseline PSA level established once they turn 50 years of age.
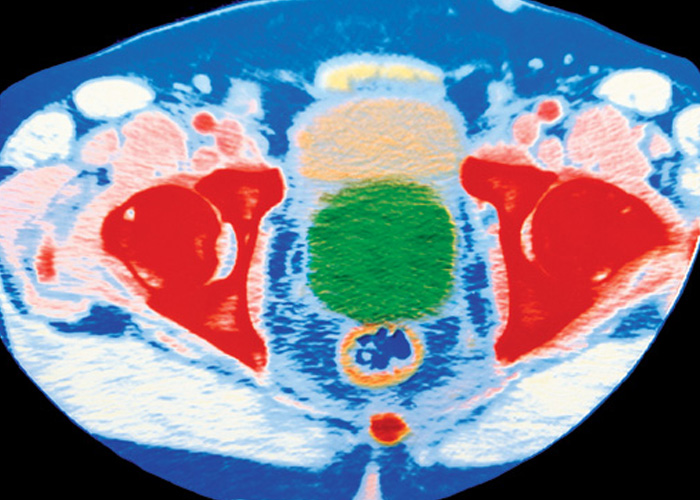
Once a cancer has been diagnosed, whether through a transrectal ultrasound, an MRI scan or a biopsy, other tests are then conducted to see if the cancer has spread within the prostate or to other parts of the body. Survival rates tend to be much higher if the disease is caught earlier and hasn’t spread further than the prostate.
Taking action over early symptoms around bladder issues is a vital first step
Treatment options and side-effects
It is vital that patients are aware of all treatment options available to them and their potential side-effects, rather than opting for the first discussed treatment. The first consultation must be open and honest, discussing all potential routes of action, not just surgery to remove the prostate, which remains in many cases the deferential treatment option.
For example, this approach (radical prostatectomy) is widely recognised as having incontinence as a significant side-effect due to damage to the nerves and muscles during the operation. Other options, such as hormone therapy and external radiotherapy, can cause similar side-effects as a biproduct of the treatment. This can go on to affect the patient long-term, including impacting on lifestyle choices, diet and exercise patterns.
By being educated on all treatment options, including brachytherapy (where radiotherapy is administered by implanting radioactive wires or grains into or close to a tumour), which has a lower incidence of severe side-effects such as impaired sexual function and incontinence, men can make more informed and knowledgeable choices of the best treatment options for them.
In order for men to have as many options available to them as possible, early diagnosis is key. Taking action over potential early symptoms around urinary and bladder issues is the vital first step.