In Clinical
Follow this topic
Bookmark
Record learning outcomes
Key facts
- Psoriasis is a complex inflammatory disease
- It is associated with significant impairment in quality of life
- Chronic plaque psoriasis accounts for up to 90 per cent of all cases
- Community pharmacists are well placed to support patients and help improve the management of their condition.
Learning objectives
After reading this feature, you should:
- Understand the possible causes and pathophysiology of plaque psoriasis
- Be able to recognise the presenting symptoms
- Know how to help patients understand and implement the best treatment
strategies for better quality of life.
Although traditionally considered to be ‘only’ a skin condition, psoriasis is now best described as a complex, multifactorial and inflammatory disease. It is thought to affect between 2 and 4 per cent of the population in Westernised countries. Patients with mild to moderate plaque psoriasis prescribed topical therapy often sub-optimally manage their condition.
Whilst it is not life-threatening, psoriasis is associated with significant impairment in quality of life, including work, family, sexual relations as well as physical and emotional well-being. The visible nature of the condition has been reported as one of its most difficult aspects.
The most common form of psoriasis, accounting for up to 90 per cent of all cases, is chronic plaque psoriasis. It affects both sexes to an equal extent and for most patients (75 per cent), psoriasis first presents between the ages of 15 and 25 years.
The remaining quarter of patients experience onset of symptoms much later in life, typically between the ages of 55 and 60.
Plaque psoriasis is characterised by well defined erythematous, silvery/white hyperkeratotic scaling plaques that classically occur on extensor surfaces of the body (e.g. elbows and knees) as well as the lower back.
In addition, in nearly 80 per cent of patients, psoriasis affects the scalp.
Often, patients with psoriasis experience changes to their nails, including abnormal nail plate growth, leading to characteristic pitting, a build-up of keratinous material underneath the nail (subungual hyperkeratosis) and detachment of the nail from its bed (onycholysis).
Psoriasis does occur, albeit less commonly, in children, where it can be misdiagnosed as atopic eczema since the scaling is less prominent and lesions often affect the face.
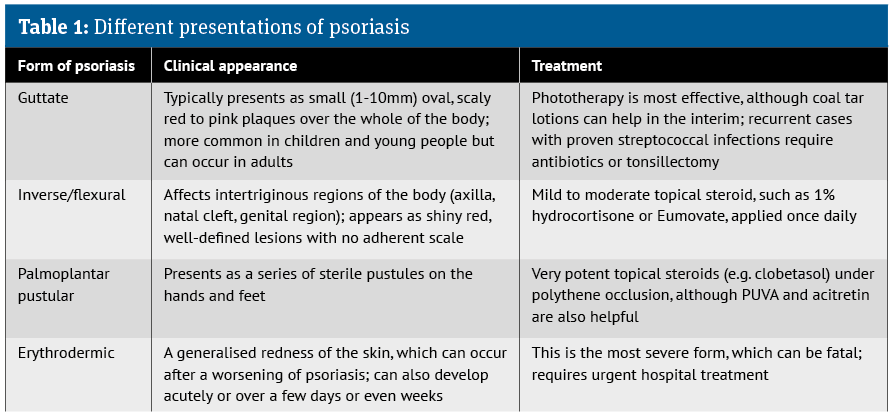
Less common forms of psoriasis are shown in Table 1, below.
Co-morbidities
Several lifestyle factors appear to be associated with psoriasis – in particular, cigarette smoking, obesity, alcohol consumption, physical inactivity and stress.
In addition, there is potential for increased risk of metabolic syndrome and cardiovascular disease, especially among patients with more severe disease.
One of the most prevalent co-morbidities is psoriatic arthritis (PsA), a chronic inflammatory, degenerative condition with progressive joint disease. Diagnosis of PsA requires assessment by a rheumatologist.
Pathophysiology
Although the precise cause of psoriasis remains unclear, it is likely that a combination of genetic, environmental and immunological factors are responsible.
Prior to the 1980s, it was believed that psoriasis was solely due to keratinocyte dysregulation, leading to hyperproliferation of these cells and the hallmark plaques.
However, in a study where patients with PsA were treated using etanercept,
a biologic agent that targets the pro-inflammatory cytokine tumour necrosis factor alpha (TNF-α), some patients also achieved significant improvement in their psoriasis.
Subsequent work has revealed how other interleukins (ILs) such as IL23 and 17A have a critical role in the disease. Indeed, many of the newer biologic treatments for the management of patients with more severe disease specifically target interleukins 12, 23 and 17.
Changes in the skin are related to alterations in the life cycle of keratinocyte cells. Under normal circumstances, keratinocytes are produced and replaced approximately every 28 days.
In psoriasis, the life cycle is reduced to around five days. Consequently, keratinocytes are produced at a much faster rate than they are shed, leading to a build-up on the surface of the skin, which is visible as the silvery white scale.
There is also an increase in the vasculature of a psoriatic plaque, and picking or scratching lesions can lead to bleeding, illustrating the underlying inflammatory component of the disease.
Genetics account for around a third of cases but there are several important triggers, including:
- Skin trauma (Koebner phenomenon): psoriasis can develop at the site of skin injury
- Climate: it is often worse during colder weather
- Infections: particularly streptococcal infections
- Antimalarial drugs, beta-blockers, NSAIDs
- Smoking, alcohol, stress.

Topical therapy
Fortunately, as many as 80 per cent of those with plaque psoriasis have mild to moderate disease that is amenable to treatment in primary care with topical therapies.
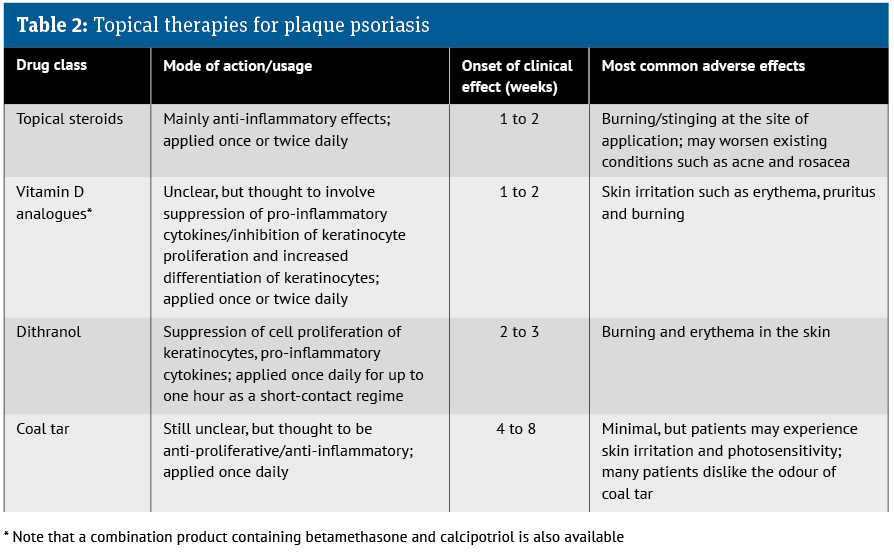
There are a number of topical agents available and a summary of these agents, their onset of action and main adverse effects are summarised in Table 2, below.
Several systematic reviews have been conducted on the efficacy of combination products containing a potent topical steroid and a vitamin D analogue, all of which have concluded that the combination therapy was more effective than either of the separate components used alone.
Consequently, guidance from NICE in 2012 recommended first-line therapy for plaque psoriasis on the trunk and limbs with “a potent corticosteroid applied once daily plus vitamin D or a vitamin D analogue applied once daily (applied separately, one in the morning and the other in the evening) for up to four weeks for adults”.
Given the risks of using potent topical steroids long-term, NICE advises that patients are reviewed after four weeks of starting treatment.
If the combination appears to be effective, the topical steroid should not be used at the same site for longer than eight weeks and treatment can be continued with the vitamin D analogue, allowing for a four-week steroid-free interval.
In contrast to the advice from NICE, the Primary Care Dermatology Society (PCDS) advocates a combination product containing betamethasone and calcipotriol (e.g. Enstilar foam), as the first- line option for plaque psoriasis on the body and scalp.
Other combination products with the same ingredients include Dovobet gel or ointment and Wynzora cream.
Emollients
While not specifically covered in clinical guidelines, emollients have an important adjunctive role to play in psoriasis, helping to soften and hydrate the stratum corneum, enhancing desquamation (shedding) of hyperkeratotic skin and providing relief of pruritus.
There is also a suggestion that emollients might improve the penetration of other topical psoriasis treatments.
Despite their widespread use in psoriasis and a BNF recommendation that these agents might be the only necessary treatment in mild psoriasis, there is a lack of robust data on the efficacy of emollients in psoriasis.
Some evidence does suggest that products containing urea or salicylic acid are beneficial. The PCDS strongly advocates the use of emollients both as soap substitutes and as a product to be left on the skin for all patients with psoriasis, alongside other active topical agents.
Emollients should be prescribed in large quantities (e.g. 500g per week for an adult and 250-500g per week for a child).
There is little objective evidence that any one emollient is superior, but patients need to find a product they find cosmetically acceptable because this will most likely improve adherence.

Secondary care treatments
- Phototherapy: involves repeated exposure to UV light, one of the oldest forms of treatment for psoriasis. It can be broadband UVB, narrow- band UVB or a combination of an oral treatment (psoralen) and UVA light, commonly referred to as PUVA. The latter is suited to patients with more widespread disease or who have failed to respond adequately to topical therapy. The most commonly used modality is narrowband UVB, which has a spectral width between 308 and 313nm because 311nm is the most effective wavelength for clearing psoriasis. However, between 60 and 75 per cent of patient using phototherapy achieve a 75 per cent improvement in disease severity, irrespective of the modality used
- Oral therapy: treatments commonly used include ciclosporin, methotrexate and acitretin. These are typically used in cases where phototherapy has been unsuccessful. Close monitoring of blood levels and other parameters such as full blood count, liver function tests, urea and electrolytes, and creatinine levels are required when taking these oral treatments, and the drug should be discontinued once clearance has been achieved
- Biological therapy: patients with the most severe level of disease are prescribed biological agents (biologics) in the management of their psoriasis. All of the available agents are monoclonal antibodies and target the activity of a range of cytokines, such as tumour necrosis factor alpha, and various interleukins, including IL12, IL17 and IL23.
How pharmacists can support patients with psoriasis
1. Ensure that all patients use an emollient for washing and moisturising. The emollient should be used over the entire body (including psoriasis areas) each day in the direction of hair growth. In practice, a good regimen is to apply the emollient around 20 to 30 minutes before any active psoriasis treatments. It is useful to be able to supply smaller tubes of the preferred emollient in addition to the monthly supply, as these can be used throughout the day and applied to any pruritic plaques.
2. Advise patients not to scratch or pick at psoriatic lesions as this can result in bleeding..
3. Advise patients to persevere with all topical psoriasis treatments because while some appear to start working within a week or two, most take up to four weeks to be effective.
4. Once a treatment starts to work, there will be a reduction in scaling. Once the skin feels flat, active treatments can be stopped and patients should only use their emollient. The plaque area will still appear to be inflamed. Advise patients that this is quite normal and it will gradually fade.
5. For some patients, maintenance therapy with Enstilar, applied twice weekly on non-consecutive days to previously affected areas, can help to reduce the number of disease flare-ups.
6. Patients with scalp psoriasis can use a de-scaling agent such as products containing salicylic acid and coconut oil overnight, and wash it out in the morning with a tar-based shampoo before applying active treatments. It is also a good idea to use a comb to remove thick scale before using active treatments.
7. Finally, it would be helpful for pharmacists to enquire as to whether any of their patients with psoriasis are experiencing back or neck pain, morning stiffness, or swollen or warm joints, as this might indicate the presence of psoriatic arthritis.
Patient support organisations
- Psoriasis Association: psoriasis-association.org.uk
- Psoriasis and Psoriatic Arthritis Alliance: papaa.org