Clinical

What’s new in COPD & asthma care (part 2)
In Clinical
Bookmark
Record learning outcomes
Part 1 in this two-part series of clinical guides looked at how COPD is diagnosed. Here we consider the role community pharmacy teams can play in its therapeutic management.
Key facts
- Management of stable COPD should be individualised based on symptoms and exacerbation risk
- Between 50 and 60 per cent of people don’t use their inhaler sufficiently well to benefit
- Pharmacists should check that the medication dose is right and discuss if a spacer would help
Â

Several drugs aid COPD management including short-acting bronchodilators, inhaled corticosteroids (ICS), long-acting beta agonists (LABA) and long-acting muscarinic agonists (LAMA).
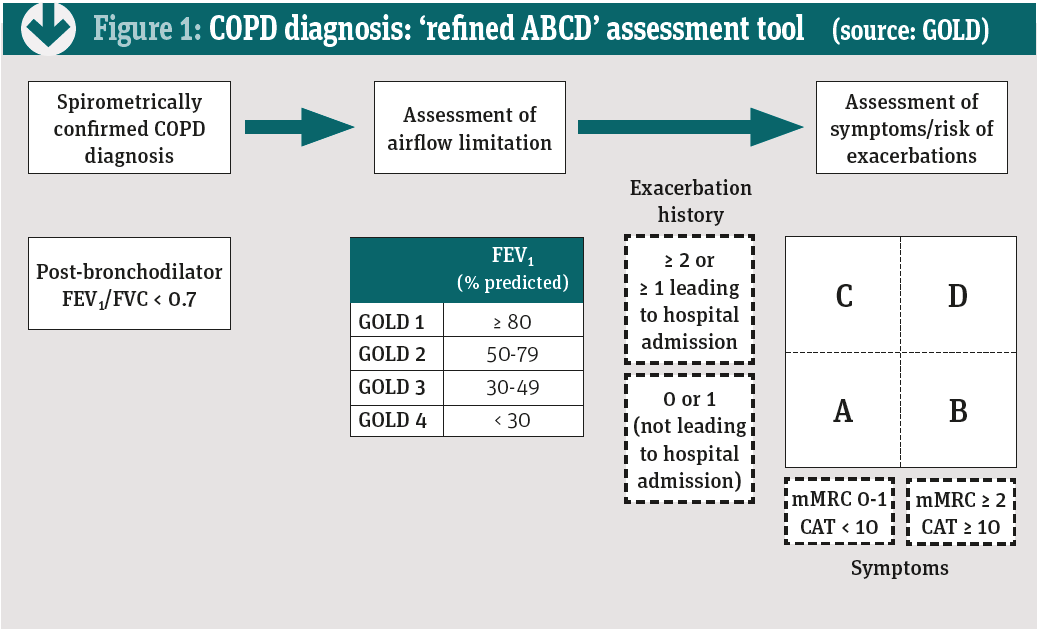
According to the Global Initiative for Chronic Obstructive Lung Disease (GOLD), which has published guidelines covering diagnosis, management and prevention since 2001, management of stable COPD should be individualised based on symptoms and exacerbation risk.
For example, patients in group B (see Figure 1) who experience persistent breathlessness while using a LABA or LAMA should receive combination treatment with both classes. No evidence supports LABA over LAMA or vice versa for initial symptomatic treatment. The choice depends on the patient’s perception of benefit.
Â
Â
In severe COPD (group D), the guidelines suggest starting with a combination of LABA plus LAMA, which seems to prevent exacerbations and improve other patient-reported outcomes more than LABA plus an ICS. However, LABA plus ICS may be the first choice for patients with a history of, or findings that suggest, an overlap between asthma and COPD. Up to 20 per cent of people with COPD also have symptoms of asthma.
As most COPD drugs are inhaled, Ashley Green, head of service development at the British Lung Foundation, says pharmacists should check a patient’s technique regularly during MUR and NMS reviews.
“There are now a large number of inhalers and pharmacists can help people find the right one for them. For instance, many people with COPD have co-morbidities, which might influence the choice. People with arthritis might not have the dexterity to use some inhalers,†he says. “Indeed, between 50 and 60 per cent of people don’t use their inhaler sufficiently well to benefit. By encouraging good inhaler technique, pharmacists can make a huge difference to patients’ health and wellbeing.â€
Check adherence
Pharmacists can also check adherence and that drugs are prescribed appropriately. “In most chronic diseases, people often stop taking treatment when they feel better, so pharmacists can help drive adherence,†Green says. “Patients might not understand the dose, what the drug does or how to administer it effectively. Unless this is explained carefully, patients can become confused.â€
Pharmacists could also check that, in line with GOLD guidance, maintenance long-acting bronchodilators have been started before discharge from hospital. Systemic corticosteroids can improve FEV1 and oxygenation, reduce recovery time and shorten hospitalisation – but treatment should not last longer than five to seven days.
When indicated, antibiotics can also hasten recovery time, reduce the risk of early relapse and treatment failure, and shorten hospitalisation. Again, treatment should last between five and seven days.
“ICS may be prescribed for mild to moderate COPD, but they can do more harm than good,†says Green. For instance, based on a Cochrane review of 43 studies, fluticasone increased non-fatal serious adverse pneumonia events (i.e. those requiring hospital admission) by a mean of 78 per cent, equivalent to 18 more cases of pneumonia per 1,000 people treated for 18 months.
Budesonide increased non-fatal serious adverse pneumonia events compared with placebo by 62 per cent, equivalent to six more cases per 1,000 people treated for nine months. However, the budesonide estimate was less precise and based on shorter studies than that for fluticasone.1
“Pharmacists should check that the dose is right and discuss whether a spacer may help,†Green says. “When there are questions in a pharmacist’s mind, they can refer the patient back to the GP and ask if this is the right prescription. On the other hand, it is also important to check that people are not stockpiling medicines, which is a waste of resources.â€
COPD is a huge problem but often simple interventions make a big difference
The BLF publishes a guide to act as a reminder when talking to patients with respiratory conditions. The guide focuses on patients’ understanding of medicines and promoting healthy lifestyles.
Preventing COPD
The GOLD guidelines note that several factors can precipitate COPD exacerbations, most commonly respiratory tract infections (RTIs), underlining the importance of pneumococcal and influenza vaccination.
A study from Imperial College, which mapped patterns of asthma and COPD across England, found that the risk of a prescription or admission for, or death from, asthma and COPD was greatest around Christmas, probably reflecting peaks in RTIs, especially influenza and respiratory syncytial virus.2 “We would encourage people to use pharmacists more to get their flu jab,†Ashley Green says.
The guidelines also underscore the importance of smoking cessation. The Liverpool Lung Project, for example, followed 8,753 people aged 45-79 years (when recruited between 1998 and 2008) until 2013. The 5,195 smokers were at higher risk of several conditions, including pneumonia (28 per cent increase), diabetes (21 per cent), CVD (45 per cent), non-lung cancers (69 per cent) and bronchitis (85 per cent). The risk of emphysema (odds ratio 5.46) and lung cancer (OR 6.0) was about six-fold higher. Smokers were also 30 per cent more likely to develop COPD.3
The GOLD guidelines identify a range of COPD risk factors, including genotype, certain congenital and developmental abnormalities, smoke from home cooking and heating fuels, and occupational exposure (e.g. dust, vapour, fumes and other chemicals).
A Canadian study of 5,176 adults aged at least 40 years reported that 6.4 per cent of never-smokers developed COPD and accounted for 27 per cent of COPD patients.4 In a study from London, black COPD patients were 44 per cent less likely to be current smokers and 4.9 times more likely to be never-smokers than white people. Ethnic differences in cigarette smoking or COPD susceptibility might account for the difference.5
The guidelines note that never-smokers who develop COPD seem to experience fewer symptoms, develop milder COPD and show less systemic inflammation.
Educating patients
In addition to raising awareness about symptoms, pharmacists can also help people with COPD understand several elements that the guidelines regard as “crucialâ€:
• The nature of COPD and factors that drive progression
• How patients and healthcare professionals can help optimise management and outcomes.
GOLD adds that patients also need general lifestyle advice – covering, for example, diet and exercise – and should be monitored for exposure to risk factors, disease progression, treatment efficacy, exacerbations, adverse events and co-morbidities.
“MURs and NMS reviews offer a great opportunity to discuss lifestyle factors, such as stopping smoking, taking exercise, participating in pulmonary rehabilitation and eating a healthy diet. People with severe COPD can find breathing takes real effort so they need more calories than healthy people. Pharmacists can also support people who are under- and overweight,†says Ashley Green.
“COPD is a huge problem but, often, simple interventions can make a big difference. Pharmacists are the heart of their communities, so they are uniquely placed to improve COPD care.â€
Â
References
1. Kew K and Seniukovich A. Inhaled steroids and risk of pneumonia for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews 2014; DOI: 10.1002/14651858.CD010115.pub2
2. Boulieri A, Hansell A and Blangiardo M. Investigating trends in asthma and COPD through multiple data sources: a small area study. Spatial and Spatio-temporal Epidemiology 2016; 19:28-36
3. Sherratt FC, Field JK and Marcus MW. Association between smoking and health outcomes in an economically deprived population: The Liverpool Lung Project.
Journal of Epidemiology and Community Health 2017; DOI: 10.1136/jech-2016-208730
4. Tan WC, Sin DD, Bourbeau J et al. Characteristics of COPD in never-smokers and
ever-smokers in the general population: Results from the CanCOLD study. Thorax 2015; 70:822-829
5. Gilkes A, Ashworth M, Schofield P et al. Does COPD risk vary by ethnicity?
A retrospective cross-sectional study. Int J Chron Obstruct Pulmon Dis 2016; 11:739-46
